Welcome to our latest blog post where we dive into the highly anticipated subject of the CMS 2026 Fee Schedule. As we approach the unveiling of the CMS 2026 Fee Schedule, it’s crucial for healthcare providers and stakeholders to stay informed and prepared for the upcoming changes. This comprehensive guide aims to equip you with the essential knowledge and insights you need to navigate through the intricacies of the new fee schedule effectively. Join us as we unravel the key updates, implications, and important details that will shape the healthcare landscape in 2026 and beyond. Let’s delve into what you need to know about the CMS 2026 Fee Schedule.
Introduction to CMS 2026 Fee Schedule
As we step into 2026, it’s crucial to stay informed about the latest updates regarding the CMS 2026 Fee Schedule. This schedule outlines the reimbursement rates and fees for various healthcare services covered by CMS (Centers for Medicare & Medicaid Services) for the year 2026.
Key Changes in the CMS 2026 Fee Schedule
One of the notable changes in the CMS 2026 Fee Schedule is the revision of reimbursement rates for telehealth services, reflecting the evolving landscape of virtual care in the healthcare industry. Additionally, there have been updates in the fee structure for preventive care services to promote overall wellness among beneficiaries.
Implications for Healthcare Providers
Healthcare providers need to familiarize themselves with the CMS 2026 Fee Schedule to ensure accurate billing and coding practices. Understanding the fee schedule can help providers optimize revenue cycle management and comply with CMS guidelines to avoid potential penalties.
Overview of CMS 2026 Fee Schedule
As we step into 2026, understanding the CMS 2026 Fee Schedule is crucial for individuals in the healthcare industry. This schedule outlines the reimbursement rates and policies set by the Centers for Medicare & Medicaid Services (CMS) for the upcoming year.
Key Updates in the CMS 2026 Fee Schedule
The CMS 2026 Fee Schedule introduces several significant changes aimed at improving healthcare delivery and ensuring fair compensation for services provided to Medicare beneficiaries. Providers can expect updates in reimbursement rates, coding guidelines, and quality reporting requirements.
Healthcare organizations need to stay abreast of these changes to adapt their billing practices and operational strategies accordingly.
Impact on Healthcare Providers
Healthcare providers will need to assess how the CMS 2026 Fee Schedule modifications will affect their revenue streams and overall financial health. The adjustments may necessitate changes in billing procedures, staff training, and resource allocation to comply with the new guidelines.
Providers should prepare for potential shifts in payment structures and patient volumes to navigate the evolving healthcare landscape effectively.
Key Changes in CMS 2026 Fee Schedule
As per the latest updates for the CMS 2026 Fee Schedule, there are significant changes that healthcare providers need to be aware of. One of the key changes is the revision in reimbursement rates for various procedures and services. These adjustments are aimed at ensuring fair compensation for providers while maintaining quality care standards.
Updated Billing Codes
The CMS 2026 Fee Schedule introduces new billing codes to accurately reflect the complexity and resources required for different medical services. Providers must familiarize themselves with these codes to ensure proper billing and reimbursement.
Quality Reporting Requirements
Another notable change is the enhanced quality reporting requirements outlined in the updated fee schedule. Providers are now required to report on additional quality metrics to receive full reimbursement for their services.
- Providers need to ensure compliance with these reporting requirements to avoid any penalties or payment reductions.
- Failure to meet the quality reporting criteria may result in a decrease in reimbursements for services rendered.
Impact of CMS 2026 Fee Schedule on Healthcare Providers
As we delve into the implications of the CMS 2026 fee schedule on healthcare providers, it’s crucial to understand the significant changes and challenges that lie ahead in the upcoming year. This fee schedule, set by the Centers for Medicare and Medicaid Services, outlines the reimbursement rates for various healthcare services and procedures, impacting providers’ revenue streams and operations.
Changes in Reimbursement Rates
One of the primary impacts of the CMS 2026 fee schedule is the changes in reimbursement rates for specific medical services. Providers may see adjustments in payment levels for procedures ranging from routine office visits to complex surgeries. It is essential for healthcare organizations to adapt to these changes to maintain financial stability.
Financial Planning and Budgeting
Healthcare providers need to proactively review their financial planning and budgeting strategies in light of the new fee schedule. Understanding the revised reimbursement rates and their effect on revenue projections is crucial for sustainable operations. Strategic financial management will be key to navigating the evolving reimbursement landscape.
Strategies for Adapting to CMS 2026 Fee Schedule
As the healthcare landscape evolves, adapting to the CMS 2026 Fee Schedule is crucial for providers to thrive. By implementing effective strategies, healthcare organizations can navigate through the changes seamlessly.
Stay Informed and Educated
Keeping up-to-date with the latest updates and changes in the CMS 2026 Fee Schedule is essential. Regularly attending training sessions and seminars can help providers understand the intricacies of the new fee schedule.
Thorough knowledge of the fee schedule can ensure accurate billing and minimize errors in claims processing.
Optimize Coding and Documentation
Efficient coding and thorough documentation are key factors in maximizing reimbursements under the CMS 2026 Fee Schedule. Providers should ensure proper coding practices and detailed documentation to support billing claims.
- Implement regular audits to identify coding discrepancies
- Train staff on proper documentation guidelines to avoid payment denials
Important Deadlines and Updates Regarding CMS 2026 Fee Schedule
As we approach the year 2026, staying informed about the CMS 2026 fee schedule is crucial for healthcare providers. Being aware of the important deadlines and updates can help streamline billing processes and ensure compliance with the latest regulations.
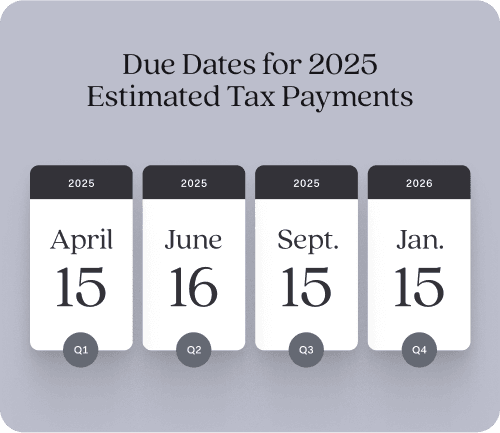
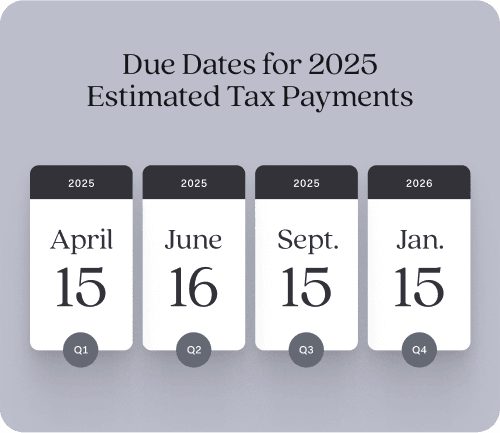
Key dates to remember
Mark your calendars for the following significant dates related to the CMS 2026 fee schedule:
- January 1, 2026: Implementation of the new fee schedule
- March 31, 2026: Deadline for providers to update their billing systems
- June 30, 2026: Last date for submitting any fee schedule appeals
Updates and Changes
For the CMS 2026 fee schedule, several updates and changes are anticipated. Providers should stay informed about:
- Revised payment rates for specific procedures
- New codes or modifiers that may impact billing
- Changes in reimbursement policies that could affect revenue
Frequently Asked Questions
- What is CMS 2026 Fee Schedule?
- The CMS 2026 Fee Schedule refers to the updated payment rates determined by the Centers for Medicare & Medicaid Services for various healthcare services provided to Medicare beneficiaries in the year 2026.
- Why is it important to understand the CMS 2026 Fee Schedule?
- Understanding the CMS 2026 Fee Schedule is crucial for healthcare providers as it directly impacts the reimbursement rates they receive for services rendered to Medicare patients. It helps providers plan their financials and operations effectively.
- What changes can we expect in the CMS 2026 Fee Schedule?
- The changes in the CMS 2026 Fee Schedule can include updates to payment rates for different medical procedures, services, and supplies. There might be adjustments based on factors like inflation, technology advancements, and healthcare policy changes.
- How can healthcare providers prepare for the changes in the CMS 2026 Fee Schedule?
- Healthcare providers can prepare for the changes in the CMS 2026 Fee Schedule by staying informed about the updates, reviewing how the changes will impact their revenue and operations, and adapting their billing and coding practices accordingly.
- Where can one access the complete CMS 2026 Fee Schedule?
- The complete CMS 2026 Fee Schedule can typically be found on the official website of the Centers for Medicare & Medicaid Services. Providers can also contact their Medicare Administrative Contractors (MACs) for more information.
Wrapping Up: Key Insights on the CMS 2026 Fee Schedule
As we conclude our deep-dive into the CMS 2026 Fee Schedule, it’s clear that healthcare providers need to stay informed and proactive to navigate the upcoming changes successfully. Understanding the nuances of the fee schedule is crucial to optimize reimbursement and ensure financial stability for your practice. By keeping abreast of the updates and modifications, you can adapt your billing processes efficiently and minimize potential disruptions.
In summary, the CMS 2026 Fee Schedule demands attention to detail and a strategic approach. Embracing technology, leveraging data analytics, and fostering strong partnerships will be vital in maximizing revenue and enhancing patient care in the evolving healthcare landscape.